2.
Fyziologické EKG
3.
EKG obraz základních patologií
4.
Poruchy srdečního rytmu - bradyarytmie
5.
Poruchy srdečního rytmu - tachyarytmie
6.
EKG u infarktu myokardu
7.
Kardiomyopatie, myokarditidy
8.
Pravostranné přetížení srdce
9.
Vrozené arytmické syndromy
10.
Ostatní (Iontové dysbalance, hypotermie a další)
11.
Kardiostimulace
Introduction
Hypokalemia is generally defined as a serum potassium level of less than 3.5 mmol/l.
The level of serum potassium is vital for regulating depolarization and repolarization of the myocardium, and hypokalemia can alter the cardiac action potential and result in abnormalities of cardiac conduction.
Moderate hypokalemia = 2.5-3.0 mmol/l
Severe hypokalemia = less than 2.5 mmol/l
Causes
Hypokalemia can result from any of the following reasons, which often occur in combination:
- inadequate intake - most common
- increased excretion
- A shift of potassium from the extracellular to the intracellular space
!! The potassium changes by 0.5 to 0.6 mmol/l with a change in pH of about 0.1!
Clinical presentation
The symptoms of hypokalemia are nonspecific and predominantly are related to muscular or cardiac function.
- often asymptomatic
- weakness and fatigue
- palpitations
- muscle cramps and pain
- psychological symptoms (psychosis, delirium, hallucinations, depression)
- worsening diabetes control or polyuria
ECG manifestation
- flattening of T waves
- T wave inversion
- U wave development - best seen in precordial leads (V2-V3)
- tall P waves and prolonged PR interval
- ST segment depression
- pseudo prolonged QT interval, because of T wave and U wave fusion (actually the QU interval with an absent T wave)
- SVT (AF, atrial flutter, atrial tachycardia)
- ventricular arrhythmias may develop (VT, VF and Torsades de Pointes)
Hypokalemia is often associated with hypomagnesaemia, which increases the risk of malignant ventricular arrhythmias.
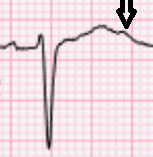
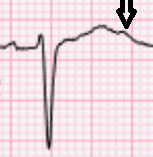
Picture 1 U wave (usually best seen in V2-V3)
ECG 1 Iatrogenic hypokalemia (flattening of T waves, U waves best seen in V1-V2, ST depressions I, V5-V6)

Management
- parenteral and oral potassium supplementation
- identification and treatment of the underlying cause
References
- Wang X, Han D, Li G. Electrocardiographic manifestations in severe hypokalemia. J Int Med Res. 2020;48(1):300060518811058. doi:10.1177/0300060518811058
- Levis JT. ECG diagnosis: hypokalemia. Perm J. 2012;16(2):57. doi:10.7812/tpp/12-015
- Eleanor Lederer, Zygimantas C Alsauskas, Lina Mackelaite, Vibha Nayak, Vecihi Batuman. Hypokalemia: Practice Essentials, Pathophysiology, Etiology. Diseases & Conditions - Medscape Reference [online]. https://emedicine.medscape.com/article/242008-overview#a1
- https://rebelem.com/r-e-b-e-l-ecg-week-4-2/

Introduction
Hypokalemia is generally defined as a serum potassium level of less than 3.5 mmol/l.
The level of serum potassium is vital for regulating depolarization and repolarization of the myocardium, and hypokalemia can alter the cardiac action potential and result in abnormalities of cardiac conduction.
Moderate hypokalemia = 2.5-3.0 mmol/l
Severe hypokalemia = less than 2.5 mmol/l
Causes
Hypokalemia can result from any of the following reasons, which often occur in combination:
- inadequate intake - most common
- increased excretion
- A shift of potassium from the extracellular to the intracellular space
!! The potassium changes by 0.5 to 0.6 mmol/l with a change in pH of about 0.1!
Clinical presentation
The symptoms of hypokalemia are nonspecific and predominantly are related to muscular or cardiac function.
- often asymptomatic
- weakness and fatigue
- palpitations
- muscle cramps and pain
- psychological symptoms (psychosis, delirium, hallucinations, depression)
- worsening diabetes control or polyuria
ECG manifestation
- flattening of T waves
- T wave inversion
- U wave development - best seen in precordial leads (V2-V3)
- tall P waves and prolonged PR interval
- ST segment depression
- pseudo prolonged QT interval, because of T wave and U wave fusion (actually the QU interval with an absent T wave)
- SVT (AF, atrial flutter, atrial tachycardia)
- ventricular arrhythmias may develop (VT, VF and Torsades de Pointes)
Hypokalemia is often associated with hypomagnesaemia, which increases the risk of malignant ventricular arrhythmias.
Picture 1 U wave (usually best seen in V2-V3)
ECG 1 Iatrogenic hypokalemia (flattening of T waves, U waves best seen in V1-V2, ST depressions I, V5-V6)

Management
- parenteral and oral potassium supplementation
- identification and treatment of the underlying cause
References
- Wang X, Han D, Li G. Electrocardiographic manifestations in severe hypokalemia. J Int Med Res. 2020;48(1):300060518811058. doi:10.1177/0300060518811058
- Levis JT. ECG diagnosis: hypokalemia. Perm J. 2012;16(2):57. doi:10.7812/tpp/12-015
- Eleanor Lederer, Zygimantas C Alsauskas, Lina Mackelaite, Vibha Nayak, Vecihi Batuman. Hypokalemia: Practice Essentials, Pathophysiology, Etiology. Diseases & Conditions - Medscape Reference [online]. https://emedicine.medscape.com/article/242008-overview#a1
- https://rebelem.com/r-e-b-e-l-ecg-week-4-2/






