2.
Fyziologické EKG
3.
EKG obraz základních patologií
4.
Poruchy srdečního rytmu - bradyarytmie
5.
Poruchy srdečního rytmu - tachyarytmie
6.
EKG u infarktu myokardu
7.
Kardiomyopatie, myokarditidy
8.
Pravostranné přetížení srdce
9.
Vrozené arytmické syndromy
10.
Ostatní (Iontové dysbalance, hypotermie a další)
11.
Kardiostimulace
Introduction
AVNRT is the most common form of regular, sustained, paroxysmal supraventricular tachycardia.
It is more likely to appear in young adults, but may be seen at any age. 70% of patients with AVNRT are females with onset at a younger age than men.
The diagnosis of AVNRT should be suspected in a patient with an abrupt onset and offset of rapid sustained palpitations, often associated with lightheadedness or dyspnea. Patients may also complain of polyuria, dizziness, chest pain and even syncope.
Causes
- The physiologic substrate for AVNRT involves dual electrical pathways in or near the AV node
- One pathway conducts rapidly and has a relatively long refractory period - the fast pathway
- The second pathway conducts relatively slowly and has a shorter refractory period - the slow pathway
- Tachycardia is initiated by a premature beat
- Both typical and atypical forms of AVNRT can result from reentry involving the fast and slow pathways
Classification
Typical AVNRT = slow-fast AVNRT
- Approximately 80 to 90% of patients with AVNRT have typical AVNRT
- This type is usually initiated by a premature atrial complex that arrives at the AV node when the fast pathway is in its refractory period. Antegrade conduction down the fast pathway is blocked and the slow pathway, with a shorter refractory period, is available for conduction to the ventricle
- As a result, the PR interval of the premature beat will be longer than those of normal beats conducted through the fast pathway.
- By the time the impulse reaches the end of the slow pathway, the fast pathway has recovered its excitability and the impulse can conduct retrogradely up the fast pathway. This creates a circuit in which the impulse goes anterogradely down the slow pathway and retrogradely up the fast pathway resulting in a sustained tachycardia.
Atypical AVNRT
- Atypical AVNRT is seen in approx. 10% of all AVNRT cases, but in some patients may coexist with the typical form
- fast-slow AVNRT - antegrade conduction can occur down the fast pathway with retrograde conduction up the slow pathway
- slow-slow AVNRT - some patients have multiple slow pathways in which both the antegrade and retrograde limbs of the circuit utilize slow AV nodal pathways
- The distinction between ‘fast-slow’ and ‘slow-slow’ forms is of no practical significance
Because of the relationships between the QRS complex and the following P wave, typical AVNRT is referred to as a "short RP tachycardia," while atypical AVNRT is a "long RP tachycardia"
Picture 1 Mechanism of AV Nodal Reentrant Tachycardia. A premature atrial complex (PAC) is conducted anterogradely through the slow pathway but is blocked at the fast pathway. The impulse activates the ventricles and at the same time is conducted retrogradely through the fast pathway to activate the atria resulting in reentry (see text). AVNRT, atrioventricular nodal reentrant tachycardia.

Basic and Bedside Electrocardiography, 1st Edition (2009)Chapter 16. Supraventricular Tachycardia due to Reentry.
ECG features
- Since this arrhythmia is usually initiated by a PAC, there is an initial ectopic atrial P wave and prolonged PR interval
- Regular narrow complex tachycardia (unless there is aberrant conduction)
- Ventricular rate is generally between 120 - 220 bpm
- ST segment depression – represents abnormalities in the repolarization
- T wave inversions following termination – in the anterior or inferior leads, immediately upon termination or may develop within the first six hours, and can persist for hours to days.
P waves in relation to QRS complexes
Typical slow-fast AVNRT
- The P wave is either hidden or is seen just emerging from the terminal part of the QRS complex > short RP interval
- Pseudo-S wave in leads II, III, and AVF
- Pseudo-R' in lead V1.
Fast-slow AVNRT
- atria are activated via the slow pathway and the P wave occurs late after the QRS complex
- P wave often appears shortly before the next QRS resembling a long RP pattern of atrial tachycardia
ECG 1 Slow-fast AVNRT
- regular narrow complex tachycardia, ventricular rate 138 bpm
- pseudo S waves in the inferior leads II, III, aVF
- discrete P waves following QRS complexes in lead V1 - pseudo R wave



ECG 2 Slow-fast AVNRT
- regular narrow complex tachycardia, ventricular rate 180 bpm
- pseudo S waves in the inferior leads II, III, aVF
- pseudo R waves in lead V1
- ST segment depression in the inferior leads – repolarization abnormality



Management
Acute therapy
- Hemodynamically unstable patient – urgent synchronized cardioversion
- Hemodynamically stable patient
Vagal manoeuvres
- Carotid sinus massage - Pressure is applied to one carotid sinus for 5 to 10 seconds. Steady pressure is recommended because it may be more reproducible. If the expected response is not obtained, the procedure is repeated on the other side after a one- to two-minute delay.
- Valsalva manoeuvres – patient is instructed to exhale forcefully against a closed glottis (against closed mouth and compressed nose) for 10 – 15s and then release.
- Modified Valsalva manoeuvre – patient does classical Valsalva manoeuvre followed by 15 seconds of passive leg raise at 45 degree angle – this may be more successful in restoring sinus rhythm.
If vagal manoeuvres are ineffective:
Adenosine
- through cardiac adenosine A1 receptor > transient AV block
- 6 mg i.v. as a rapid bolus with saline flush
- second dose – 12 mg i.v., safe within 1 min of the last dose
- maximum dose = 18 mg
If vagal manoeuvres and adenosine are ineffective:
Beta blockers or calcium channel blockers
Synchronized DC cardioversion
- is recommended when drug therapy fails to convert or control the tachycardia.
Chronic therapy
- Patients with minimal symptoms and infrequent episodes of tachycardia can be followed-up without the need for ablation or long-term pharmacological therapy
- Approximately one-half of them may become asymptomatic within the next 13 years
- Catheter ablation is recommended for symptomatic, recurrent AVNRT
- Diltiazem or verapamil in patients without HFrEF, or beta-blockers should be considered if ablation is not an option
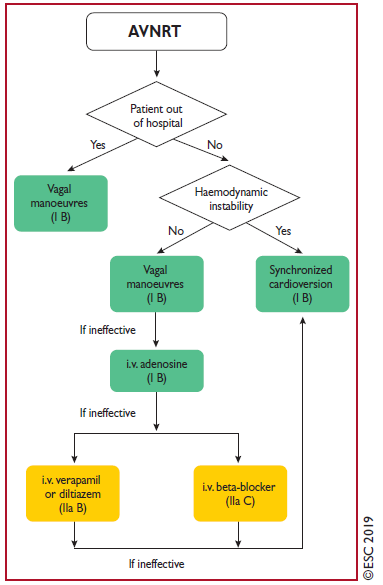
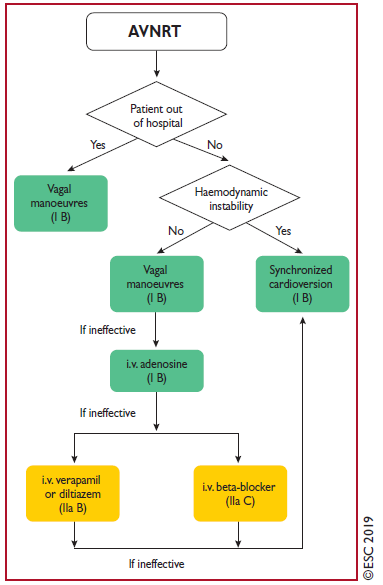
Picture 2 AVNRT treatment as per ESC guidelines
References
- CAMM, A. J., LÜSCHER, T. F., & SERRUYS, P. W. (2009). The ESC textbook of cardiovascular medicine. Oxford, Oxford University Press
- Josep Brugada, Demosthenes G Katritsis, Elena Arbelo, Fernando Arribas, Jeroen J Bax, Carina Blomström-Lundqvist, Hugh Calkins, Domenico Corrado, Spyridon G Deftereos, Gerhard-Paul Diller, Juan J Gomez-Doblas, Bulent Gorenek, Andrew Grace, Siew Yen Ho, Juan-Carlos Kaski, Karl-Heinz Kuck, Pier David Lambiase, Frederic Sacher, Georgia Sarquella-Brugada, Piotr Suwalski, Antonio Zaza, ESC Scientific Document Group, 2019 ESC Guidelines for the management of patients with supraventricular tachycardia The Task Force for the management of patients with supraventricular tachycardia of the European Society of Cardiology (ESC): Developed in collaboration with the Association for European Paediatric and Congenital Cardiology (AEPC), European Heart Journal, Volume 41, Issue 5, 1 February 2020, Pages 655–720, https://doi.org/10.1093/eurheartj/ehz467
- Bradley P Knight, MD, FACC (2020). Atrioventricular nodal reentrant tachycardia In I. Susan B Yeon, MD, JD, FACC (Ed.), UpToDate. Retrieved February 5, 2021 from https://www-uptodate-com.ezproxy.is.cuni.cz/contents/atrioventricular-nodal-reentrant-tachycardia?search=atrioventricular%20nodal&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1
- Strauss, David G., et al. Marriott's Practical Electrocardiography. Wolters Kluwer, 2021
Picture 1: Basic and Bedside Electrocardiography, 1st Edition (2009)Chapter 16. Supraventricular Tachycardia due to Reentry. Accessible at https://doctorlib.info/cardiology/electrocardiography/17.html
Picture 2 : Acute therapy of atrioventricular nodal reentrant tachycardia. (2019). [Graph]. Accessible at: https://academic.oup.com/eurheartj/article/41/5/655/5556821

Introduction
AVNRT is the most common form of regular, sustained, paroxysmal supraventricular tachycardia.
It is more likely to appear in young adults, but may be seen at any age. 70% of patients with AVNRT are females with onset at a younger age than men.
The diagnosis of AVNRT should be suspected in a patient with an abrupt onset and offset of rapid sustained palpitations, often associated with lightheadedness or dyspnea. Patients may also complain of polyuria, dizziness, chest pain and even syncope.
Causes
- The physiologic substrate for AVNRT involves dual electrical pathways in or near the AV node
- One pathway conducts rapidly and has a relatively long refractory period - the fast pathway
- The second pathway conducts relatively slowly and has a shorter refractory period - the slow pathway
- Tachycardia is initiated by a premature beat
- Both typical and atypical forms of AVNRT can result from reentry involving the fast and slow pathways
Classification
Typical AVNRT = slow-fast AVNRT
- Approximately 80 to 90% of patients with AVNRT have typical AVNRT
- This type is usually initiated by a premature atrial complex that arrives at the AV node when the fast pathway is in its refractory period. Antegrade conduction down the fast pathway is blocked and the slow pathway, with a shorter refractory period, is available for conduction to the ventricle
- As a result, the PR interval of the premature beat will be longer than those of normal beats conducted through the fast pathway.
- By the time the impulse reaches the end of the slow pathway, the fast pathway has recovered its excitability and the impulse can conduct retrogradely up the fast pathway. This creates a circuit in which the impulse goes anterogradely down the slow pathway and retrogradely up the fast pathway resulting in a sustained tachycardia.
Atypical AVNRT
- Atypical AVNRT is seen in approx. 10% of all AVNRT cases, but in some patients may coexist with the typical form
- fast-slow AVNRT - antegrade conduction can occur down the fast pathway with retrograde conduction up the slow pathway
- slow-slow AVNRT - some patients have multiple slow pathways in which both the antegrade and retrograde limbs of the circuit utilize slow AV nodal pathways
- The distinction between ‘fast-slow’ and ‘slow-slow’ forms is of no practical significance
Because of the relationships between the QRS complex and the following P wave, typical AVNRT is referred to as a "short RP tachycardia," while atypical AVNRT is a "long RP tachycardia"
Picture 1 Mechanism of AV Nodal Reentrant Tachycardia. A premature atrial complex (PAC) is conducted anterogradely through the slow pathway but is blocked at the fast pathway. The impulse activates the ventricles and at the same time is conducted retrogradely through the fast pathway to activate the atria resulting in reentry (see text). AVNRT, atrioventricular nodal reentrant tachycardia.

Basic and Bedside Electrocardiography, 1st Edition (2009)Chapter 16. Supraventricular Tachycardia due to Reentry.
ECG features
- Since this arrhythmia is usually initiated by a PAC, there is an initial ectopic atrial P wave and prolonged PR interval
- Regular narrow complex tachycardia (unless there is aberrant conduction)
- Ventricular rate is generally between 120 - 220 bpm
- ST segment depression – represents abnormalities in the repolarization
- T wave inversions following termination – in the anterior or inferior leads, immediately upon termination or may develop within the first six hours, and can persist for hours to days.
P waves in relation to QRS complexes
Typical slow-fast AVNRT
- The P wave is either hidden or is seen just emerging from the terminal part of the QRS complex > short RP interval
- Pseudo-S wave in leads II, III, and AVF
- Pseudo-R' in lead V1.
Fast-slow AVNRT
- atria are activated via the slow pathway and the P wave occurs late after the QRS complex
- P wave often appears shortly before the next QRS resembling a long RP pattern of atrial tachycardia
ECG 1 Slow-fast AVNRT
- regular narrow complex tachycardia, ventricular rate 138 bpm
- pseudo S waves in the inferior leads II, III, aVF
- discrete P waves following QRS complexes in lead V1 - pseudo R wave



ECG 2 Slow-fast AVNRT
- regular narrow complex tachycardia, ventricular rate 180 bpm
- pseudo S waves in the inferior leads II, III, aVF
- pseudo R waves in lead V1
- ST segment depression in the inferior leads – repolarization abnormality



Management
Acute therapy
- Hemodynamically unstable patient – urgent synchronized cardioversion
- Hemodynamically stable patient
Vagal manoeuvres
- Carotid sinus massage - Pressure is applied to one carotid sinus for 5 to 10 seconds. Steady pressure is recommended because it may be more reproducible. If the expected response is not obtained, the procedure is repeated on the other side after a one- to two-minute delay.
- Valsalva manoeuvres – patient is instructed to exhale forcefully against a closed glottis (against closed mouth and compressed nose) for 10 – 15s and then release.
- Modified Valsalva manoeuvre – patient does classical Valsalva manoeuvre followed by 15 seconds of passive leg raise at 45 degree angle – this may be more successful in restoring sinus rhythm.
If vagal manoeuvres are ineffective:
Adenosine
- through cardiac adenosine A1 receptor > transient AV block
- 6 mg i.v. as a rapid bolus with saline flush
- second dose – 12 mg i.v., safe within 1 min of the last dose
- maximum dose = 18 mg
If vagal manoeuvres and adenosine are ineffective:
Beta blockers or calcium channel blockers
Synchronized DC cardioversion
- is recommended when drug therapy fails to convert or control the tachycardia.
Chronic therapy
- Patients with minimal symptoms and infrequent episodes of tachycardia can be followed-up without the need for ablation or long-term pharmacological therapy
- Approximately one-half of them may become asymptomatic within the next 13 years
- Catheter ablation is recommended for symptomatic, recurrent AVNRT
- Diltiazem or verapamil in patients without HFrEF, or beta-blockers should be considered if ablation is not an option
Picture 2 AVNRT treatment as per ESC guidelines
References
- CAMM, A. J., LÜSCHER, T. F., & SERRUYS, P. W. (2009). The ESC textbook of cardiovascular medicine. Oxford, Oxford University Press
- Josep Brugada, Demosthenes G Katritsis, Elena Arbelo, Fernando Arribas, Jeroen J Bax, Carina Blomström-Lundqvist, Hugh Calkins, Domenico Corrado, Spyridon G Deftereos, Gerhard-Paul Diller, Juan J Gomez-Doblas, Bulent Gorenek, Andrew Grace, Siew Yen Ho, Juan-Carlos Kaski, Karl-Heinz Kuck, Pier David Lambiase, Frederic Sacher, Georgia Sarquella-Brugada, Piotr Suwalski, Antonio Zaza, ESC Scientific Document Group, 2019 ESC Guidelines for the management of patients with supraventricular tachycardia The Task Force for the management of patients with supraventricular tachycardia of the European Society of Cardiology (ESC): Developed in collaboration with the Association for European Paediatric and Congenital Cardiology (AEPC), European Heart Journal, Volume 41, Issue 5, 1 February 2020, Pages 655–720, https://doi.org/10.1093/eurheartj/ehz467
- Bradley P Knight, MD, FACC (2020). Atrioventricular nodal reentrant tachycardia In I. Susan B Yeon, MD, JD, FACC (Ed.), UpToDate. Retrieved February 5, 2021 from https://www-uptodate-com.ezproxy.is.cuni.cz/contents/atrioventricular-nodal-reentrant-tachycardia?search=atrioventricular%20nodal&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1
- Strauss, David G., et al. Marriott's Practical Electrocardiography. Wolters Kluwer, 2021
Picture 1: Basic and Bedside Electrocardiography, 1st Edition (2009)Chapter 16. Supraventricular Tachycardia due to Reentry. Accessible at https://doctorlib.info/cardiology/electrocardiography/17.html
Picture 2 : Acute therapy of atrioventricular nodal reentrant tachycardia. (2019). [Graph]. Accessible at: https://academic.oup.com/eurheartj/article/41/5/655/5556821






